Written by: Emmanuel Dubure, MPhil & Kristen DiFilippo, PhD, RDN
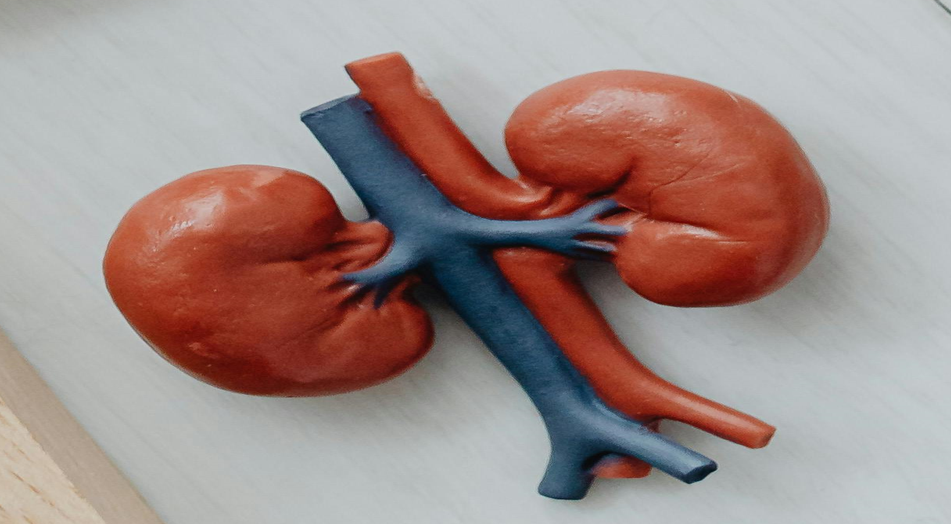
Chronic Kidney Disease (CKD) occurs when the kidneys lose their ability to function properly over time (Pan American Health Organization, 2022). The kidneys, a pair of organs that remove waste substances from the body, also perform other functions including controlling blood pressure and helping to make red blood cells (Raghavendra et al., 2013). When the kidneys fail to work properly, waste can build up in the body and cause harm including cardiovascular disease and kidney failure as well as anemia, weak bones, fluid retention, and the accumulation of unwanted substances in the blood (Bello et al., 2017). CKD impacts many people with over 800 million people suffering CKD globally (Kovesdy, 2022), and nearly 36 million in the United States (Centers for Disease Control and Prevention[CDC], 2023).
Diagnosis of CKD
CKD is diagnosed when the glomerular filtration rate (GFR), a marker of kidney function declines to less than 60 mL/min, or when GFR is above 60 mL/min with other signs of kidney abnormality for at least three months. The signs used with GFR to diagnose CKD include high protein levels in the urine and structural changes in the kidneys which can be assessed by viewing the kidneys in a medical scan.
Stages of CKD
There are five stages of CKD. These are classified based on the extent of decline of kidney function.
- Stage 1: A normal GFR of ≥ 90 mL/min, but with other signs of kidney abnormality such as high protein in the urine
- Stage 2: A mild decrease in kidney function and a GFR of 60–89 mL/min with other signs of kidney abnormality
- Stage 3a: A moderate decline in kidney function with a GFR of 45–59 mL/min
- Stage 3b: A moderate decline in kidney function with a GFR of 30–44 mL/min
- Stage 4: A severe decline in kidney function with a GFR of 15–29 mL/min
- Stage 5: Also known as end-stage kidney disease and characterized by a GFR of <15 mL/min
(Kidney Disease: Improving Global Outcomes [KDIGO], 2014)
Signs and symptoms of CKD
The initial stages of CKD may show no visible signs (Chen et al., 2019). However, some later signs may include tiredness, itchy skin, puffiness, swollen limbs, muscle cramps, and changes in urine output and appearance (National Kidney Foundation, 2024).
Risk factors for CKD
Risk factors for CKD include uncontrolled diabetes, hypertension and advancing age. Other factors include smoking, obesity, a family history of CKD and being Black/African American. Excessive use of certain medications, autoimmune conditions and some infections may also affect the kidneys (Evans & Taal, 2015).
Prevention of CKD
CKD can be prevented by managing pre-existing medical conditions and risk factors for the disease. It is recommended to maintain a healthy weight, avoid smoking and eat a diet low in sodium, saturated fats and trans fats (National Institute of Diabetes and Digestive and Kidney Diseases, 2024).
Management of CKD
CKD is managed using dietary modification, medication and dialysis.
- Dietary changes: People with CKD will need a special diet to reduce the buildup of waste in the body. Protein, sodium, potassium and phosphorus intake is often controlled with the help of a dietitian (Kalantar-Zadeh & Fouque, 2017). Fluids may also be restricted depending on the patient’s condition (Lambert et al., 2022).
- Medication: Medication may be used to treat comorbidities such as diabetes and heart disease (Li et al., 2023).
- Dialysis: End-stage kidney disease is managed with dialysis, a procedure to artificially remove waste from the blood (Himmelfarb et al., 2020). Patients may also need a kidney transplant to survive (Hariharan et al., 2021).
CKD is a progressive disease with many adverse outcomes. Prevention, early diagnosis, and treatment are crucial to reduce the burden of this disease.
References
Bello, A. K., Alrukhaimi, M., Ashuntantang, G. E., Basnet, S., Rotter, R. C., Douthat, W. G., Kazancioglu, R., Köttgen, A., Nangaku, M., Powe, N. R., White, S. L., Wheeler, D. C., & Moe, O. (2017). Complications of chronic kidney disease: current state, knowledge gaps, and strategy for action. Kidney International Supplements, 7(2), 122–129. https://doi.org/10.1016/j.kisu.2017.07.007
Centers for Disease Control and Prevention. (2023). Chronic Kidney Disease in the United States, 2023. https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html
Chen, T. K., Knicely, D. H., & Grams, M. E. (2019). Chronic Kidney Disease Diagnosis and Management: A Review. JAMA, 322(13), 1294–1304. https://doi.org/10.1001/jama.2019.14745
Damtie, S., Biadgo, B., Baynes, H. W., Ambachew, S., Melak, T., Asmelash, D., & Abebe, M. (2018). Chronic Kidney Disease and Associated Risk Factors Assessment among Diabetes Mellitus Patients at A Tertiary Hospital, Northwest Ethiopia. Ethiopian Journal of Health Sciences, 28(6), 691–700. https://doi.org/10.4314/ejhs.v28i6.3
Evans, P. D., & Taal, M. W. (2015). Epidemiology and causes of chronic kidney disease. Medicine (United Kingdom), 43(8), 450–453. https://doi.org/10.1016/j.mpmed.2015.05.005
Hariharan, S., Israni, A. K., & Danovitch, G. (2021). Long-Term Survival after Kidney Transplantation. The New England Journal of Medicine, 385(8), 729–743. https://doi.org/10.1056/NEJMra2014530
Himmelfarb, J., Vanholder, R., Mehrotra, R., & Tonelli, M. (2020). The current and future landscape of dialysis. Nature Reviews Nephrology, 16(10), 573–585. https://doi.org/10.1038/s41581-020-0315-4
Kalantar-Zadeh, K., & Fouque, D. (2017). Nutritional Management of Chronic Kidney Disease. New England Journal of Medicine, 377(18), 1765–1776. https://doi.org/10.1056/NEJMra1700312
Kazancioğlu, R. (2013). Risk factors for chronic kidney disease: an update. Kidney International Supplements, 3(4), 368–371. https://doi.org/10.1038/kisup.2013.79
Kidney Disease: Improving Global Outcomes (KDIGO). (2014). KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. IFAC Proceedings Volumes (IFAC-PapersOnline), 19(1), 4477–4483. https://doi.org/10.3182/20140824-6-za-1003.01333
Kovesdy, C. P. (2022). Epidemiology of chronic kidney disease: an update 2022. Kidney International Supplements, 12(1), 7–11. https://doi.org/10.1016/j.kisu.2021.11.003
Lambert, K., Neale, E., Nichols, L., Brauer, D., Blomfield, R., Caurana, L., Isautier, J., Jesudason, S., & Webster, A. C. (2022). Interventions for improving adherence to dietary salt and fluid restrictions in people with chronic kidney disease (stage 4 and 5). In The Cochrane Database of Systematic Reviews (Vol. 2022, Issue 10). https://doi.org/10.1002/14651858.CD015181
Li, Y., Barve, K., Cockrell, M., Agarwal, A., Casebeer, A., Dixon, S. W., & Poonawalla, I. (2023). Managing comorbidities in chronic kidney disease reduces utilization and costs. BMC Health Services Research, 23(1), 1418. https://doi.org/10.1186/s12913-023-10424-8
National Institute of Diabetes and Digestive and Kidney Diseases. (2024). Preventing Chronic Kidney Disease. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd/prevention
National Kidney Foundation. (2024). 10 Signs You May Have Kidney Disease. https://www.kidney.org/news/ekidney/august14/10_Signs_You_May_Have_Kidney_Disease
Pan American Health Organization. (2022). Chronic kidney disease. https://www.paho.org/en/topics/chronic-kidney-disease
Raghavendra, Mallikarjun, & Vidya, M. . (2013). Functions of kidney & artificial kidneys. International Journal of Innovative Research in Electrical, Electronics, Instrumentation and Control Engineering, 1(1), 1–5.
Ruggenenti, P., Cravedi, P., & Remuzzi, G. (2012). Mechanisms and Treatment of CKD. Journal of the American Society of Nephrology, 23(12), 1917–1928. https://doi.org/10.1681/ASN.2012040390
Photo credit: Karolina Grabowska via Pexels